Cervicogenic headache: when headaches originate from the neck
- Charbel Jean KORTBAWI DO, MSc.

- Sep 1, 2025
- 3 min read
What is cervicogenic headache?
Headache originating in the cervical spine
Cervicogenic headache (or CC) is a type of headache caused by dysfunction of the cervical structures (vertebrae, intervertebral discs, muscles, joints). Although it was first described in the 1920s, it was not really recognised until the end of the 20th century thanks to the work of Professor Sjaastad.
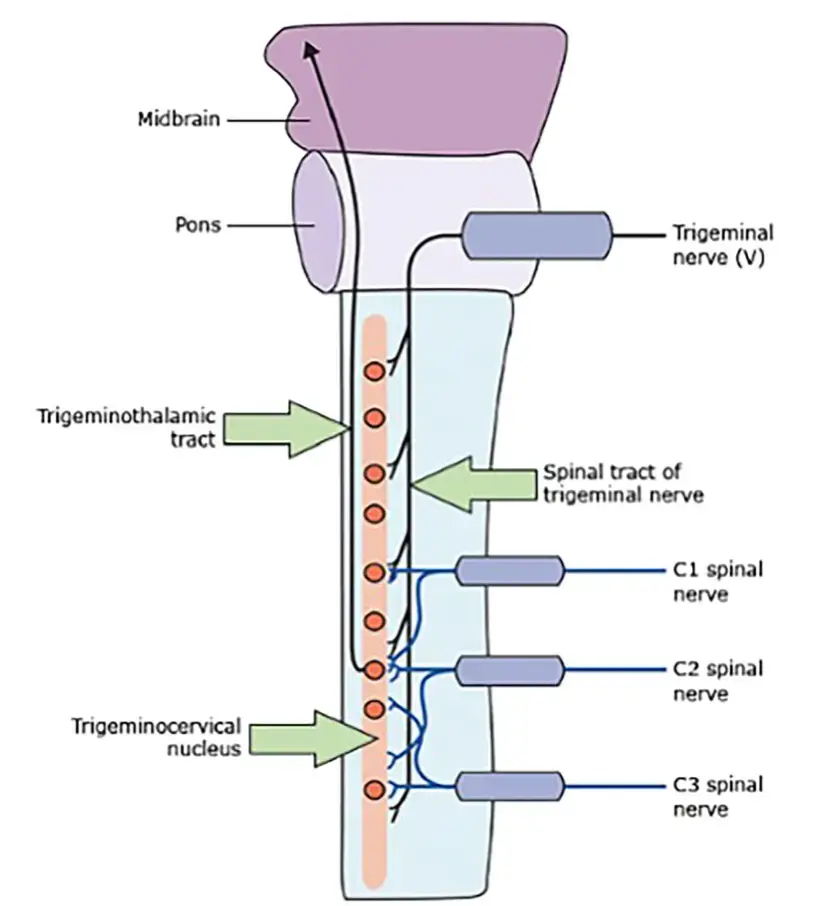
This particular type of headache originates from the convergence of the cervical nerves and the trigeminal nerve at the brainstem, a phenomenon known as trigeminal-cervical convergence. This explains why the symptoms can resemble a migraine, sometimes leading to misdiagnosis.

Characteristic symptoms
The characteristic signs of cervicogenic headache include:
Unilateral, fixed pain, often located at the back of the skull, sometimes radiating to the forehead or eye.
Reduced cervical mobility, particularly in rotation.
Pain that worsens with certain neck movements or prolonged posture.
Sensitivity to palpation of the neck muscles and joints, particularly at C1-C2.
Sometimes, associated symptoms similar to migraine: nausea, photophobia, phonophobia, dizziness.
The duration of episodes varies greatly, from a few hours to several days, and the frequency can range from a few attacks per year to several per week.
Differential diagnosis
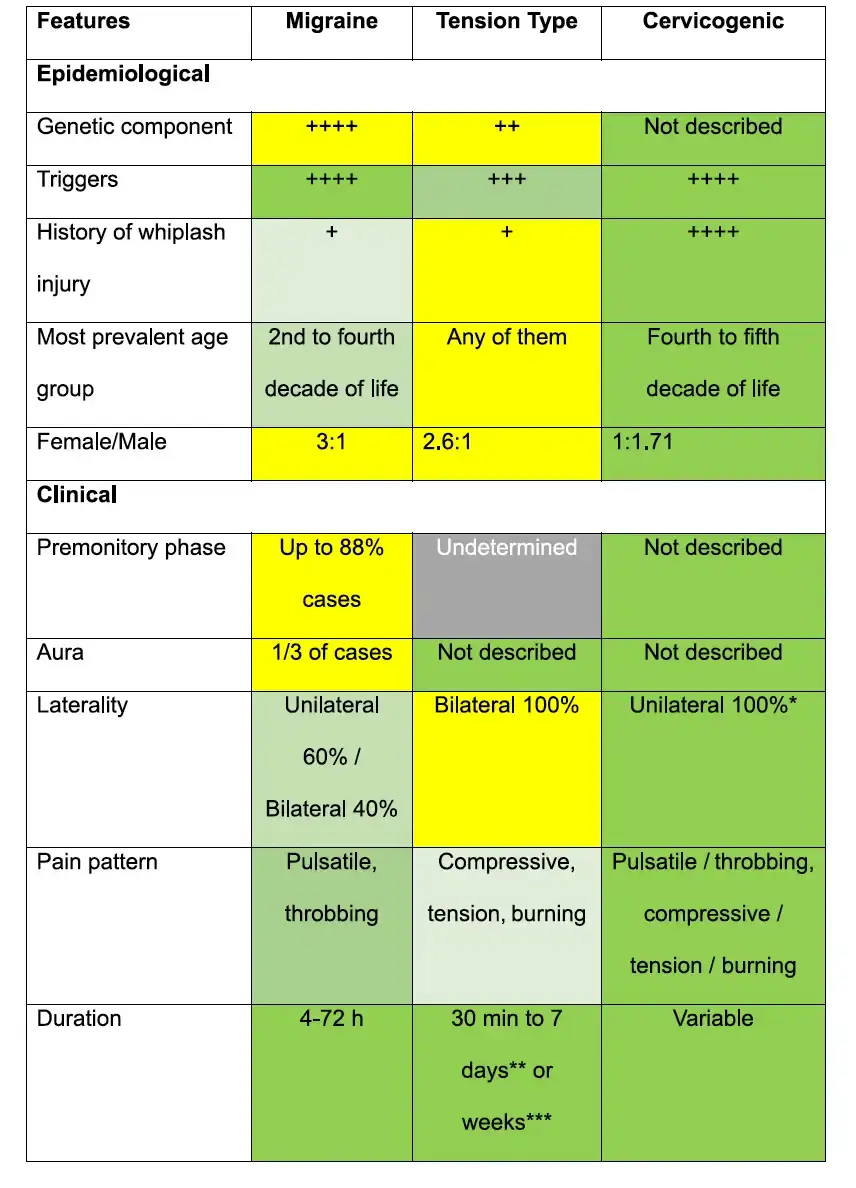
Distinguishing cervicogenic headache from migraine or tension headache is a clinical challenge. Diagnosis is based on:
A targeted physical examination of the cervical spine.
The cervical flexion-rotation test, which is often limited in CC.
Clinical criteria defined by the International Headache Society (IHS) and the CHISG (Cervicogenic Headache International Study Group), including unilateral pain, loss of cervical mobility and triggering by local pressure.
Improvement in symptoms after anaesthetic block of the cervical nerves, particularly C2-C3.
Common causes of cervicogenic hedaches
The most common causes include:
Cervical trauma (whiplash, falls, etc.)
Cervical osteoarthritis
Postural disorders (working at a computer screen, postural stress)
Joint dysfunction at C2-C3 or C1-C2
Cervical musculoskeletal disorders
Cervicogenic headache treatment
The treatment of cervicogenic headache is based on a multimodal approach:
Osteopathy and physiotherapy
A scientific article published in May 2025 in Frontiers in Neurology, entitled ‘Comparative safety and efficacy of manual therapy interventions for cervicogenic headache: a systematic review and network meta-analysis’, compares the effectiveness of different manual therapy techniques in the treatment of cervicogenic headaches, a disorder for which these approaches remain among the most effective and least invasive.
Joint mobilisation techniques are particularly effective in reducing pain, improving cervical mobility and reducing functional disability. These benefits are both significant and long-lasting. Cervical spinal manipulation, on the other hand, appears to be the most effective short-term intervention for relieving pain and restoring function, provided it is performed by an experienced professional. Gentle mobilisation and massage offer safe options, particularly for patients with contraindications to manipulation.
In summary, osteopathy and manual therapy have a place in the management of cervicogenic headaches, helping to improve cervical mobility, rebalance muscle tension and relieve pain. Several studies show that exercises targeting the deep muscles of the neck, combined with mobilisation techniques, can reduce the intensity and frequency of headaches in the long term.
Anaesthetic block
A diagnostic test, but also a therapeutic option, involves the infiltration of lidocaine or corticosteroids into the cervical joints or the greater occipital nerve.
Pulsed radiofrequency and surgery
If conservative treatments fail, techniques such as radiofrequency at the cervical nerves or decompression surgery may be considered in very specific cases.
Conclusion
Cervicogenic headache is an underestimated cause of chronic headaches. A thorough clinical examination, combined with manual and functional management, can often provide lasting relief. As an osteopath specialising in chronic pain and cervical pathologies, I offer an individualised approach, incorporating the latest recommendations based on scientific data.
Charbel Jean Kortbawi DO, MSc.
Ostéopathe à Paris
Diplôme Français d'ostéopathie (DO)
Master 2 Neurosciences du mouvement
Diplôme Universitaire Gestion de douleur chronique
Diplôme Universitaire Douleur et motricité humaine
Diplôme Universitaire Anatomie clinique et imagerie


Comments